
|
|
Introduction
“Employment in health care is projected to grow faster than the average for all occupations through 2032 with 1.8 million openings per year,” according to the U.S. Department of Labor.
The growing demand for health care workers is quickly outpacing the ability to fill positions due to talent shortages, burnout among health care workers, and increasing skill demands.
Communities in North Carolina, particularly rural ones, are challenged with not only providing quality health care but also supplying the local health care workforce.
One area of major concern is the demand for nurses — both registered nurses (RNs) and licensed practical nurses (LPNs).
Over the next decade, hospitals are projected to face the largest shortage of (RNs), followed by nursing homes, extended care, and assisted living facilities. Similarly, nursing homes, extended care, and assisted living facilities could see a 50% projected shortage of LPNs and hospitals as much as 31.7% by 2033.
As these nursing shortages loom, organizations across the state are finding creative solutions to address the critical workforce needs in their communities.
The following case study explores the partnership between Craven Community College and CarolinaEast Health System to address their community’s health care workforce challenges.
Understanding Craven County
Some of the sickest populations in the country tend to be those living in rural areas. The NC Rural Center considers 78 of North Carolina’s 100 counties rural. These counties are home to 40% of the state’s population, making North Carolina’s rural population the second largest in the country behind Texas.
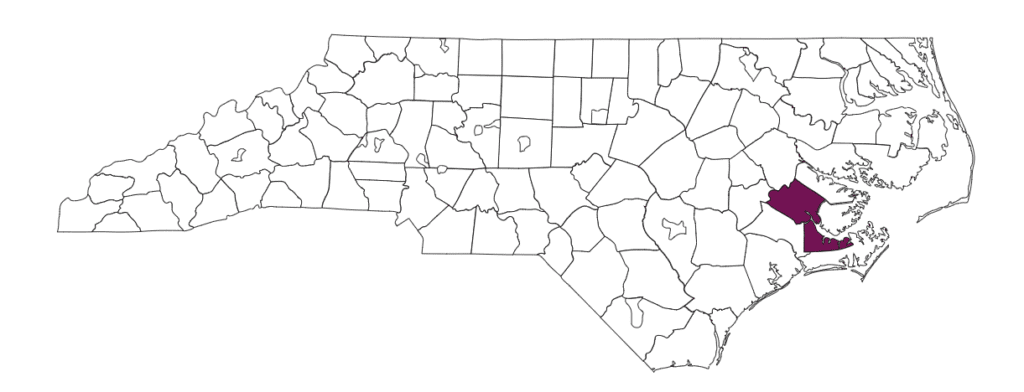
Craven Community College and CarolinaEast Health System are situated in Craven County, a rural eastern county on the Neuse River with New Bern as its county seat. According to the 2020 U.S. Census, Craven County has a population of 100,700. As of 2023, 17.6% of Craven County’s population is below the poverty level, and Craven’s older population, made up of individuals 65 years and older, is 21.7% compared to 17.7% in North Carolina. Veterans account for 12.6% of the county’s population — one of the highest veteran populations in the state.
Cancer and heart disease are the top two leading causes of death among Craven County residents, according to a 2023 county health report. Other unintentional injuries, including drug overdose deaths, is the third leading cause of death.
In a 2021 community health needs assessment report, behavioral health, community wellness, and workforce development were identified as the top three health priorities for 2022-2024.
The rising health care needs of community members continue to strain the health care system. As in many communities across North Carolina, there are not enough trained health care workers to meet the health care needs of the county.
Searching for a solution
CarolinaEast Health System is a multi-facility health care provider and includes a 350-bed inpatient hospital, comprehensive cancer center, surgery center, rehabilitation hospital, and more. The system is the county’s second largest employer.
In 2018, leaders from CarolinaEast approached Craven Community College about the system’s need for a robust talent pipeline of nurses.
One solution: Expand the college’s nursing program, admitting more students each year.
The challenge: More nursing students require more nursing faculty.
The North Carolina Board of Nursing (NCBON) sets a 10:1 student-faculty ratio for clinical experiences. To expand the college’s nursing program and admit more students, they would need to hire an additional nursing faculty member, which would cost the college money they did not have.
Most of the funding for North Carolina’s community colleges comes from state appropriations and is based on a funding formula with the largest factor being the number of full-time equivalent (FTE) students. Colleges receive funding in proportion to the number of FTE students enrolled in each of their programs. Courses that are more expensive to offer and considered higher workforce priorities receive more funding than others based on a four-tier model.
Colleges are funded in arrears, which means they are funded based on the current year’s FTE or an average of the previous two years’ FTE. This makes it difficult for colleges to start or expand programs, particularly those with high startup costs, since they only receive funding for the program after it generates FTE.
When CarolinaEast approached Craven Community College in 2018 about the need for more nurses, leaders from the two institutions devised a solution: CarolinaEast would put up the initial funding the college needed to hire a nursing instructor and grow their program. Then, once the program started and enrolled students, the FTE those students generated would pay for the nursing instructor.
In 2019, CarolinaEast awarded a $150,000 grant to Craven Community College, which allowed the college to hire a full-time nursing instructor and expand their nursing program.
More on community college funding:
In the 2023-25 biennium budget, North Carolina’s legislature allocated nonrecurring funding to help community colleges start up or expand “programs in high-demand healthcare careers that require significant start-up funds.” For the start up funding, colleges can apply for funding for one program each fiscal year, and they have to match a percentage of the total cost of the program based on FTE.
In 2024, the North Carolina Community College System (NCCCS) proposed a new funding model called Propel NC. Under this proposed model, colleges would still receive state funding based on FTE, but the current FTE tiers would shift to “workforce sectors” with courses ranked and valued by statewide salary job demand data every three years. All curriculum and continuing education (CE) courses would be housed in the same workforce sector, so a nursing curriculum and nursing CE course would be funded the same way.
The NCCCS requested nearly $100 million from the General Assembly this short session to implement Propel NC. While both legislative chambers included some initial funding for the model in their budget proposals, the General Assembly adjourned before passing an adjustment budget.
The mini budget passed by lawmakers and vetoed by Gov. Cooper in September did not include that funding for Propel NC. At the September State Board of Community Colleges meeting, NCCCS leaders said they are continuing advocacy efforts for Propel NC and preparing to implement the model should they receive the funding to do so.
Growing Craven Community College’s nursing program
The $150,000 grant from CarolinaEast paid the salary and benefits for one full-time nursing instructor for two years. This initial investment allowed Craven Community College to add 16 seats to their associate degree in nursing (ADN) program, expanding the program from 48 students to 64 students. The college also added six seats to their licensed practical nursing (LPN) program, growing the program from 10 students to 16.
After the success of the initial two-year grant, CarolinaEast awarded the college a second two-year grant of $336,000, which paid the salaries and benefits of two full-time and one part-time nursing instructors for two years.
With this second round of funding, Craven Community College expanded its nursing program again by introducing a spring entry cohort for their ADN program in 2023. Previously, the college only offered student entry in the fall. Adding a spring cohort allowed the college to admit 32 ADN students in the fall and 32 ADN students in the spring.
The college also added eight seats in each cohort for transition students — those transitioning from LPN to ADN — meaning Craven Community College could graduate 80 ADN students each year.
In addition to funding, CarolinaEast provided clinical training space for Craven Community College’s nursing students. To do so, CarolinaEast reconfigured their existing space, adding two additional clinical units to accommodate the growth.

Results
The grants from CarolinaEast allowed Craven Community College to expand their ADN and LPN programs, and while there was some attrition — not every student who started the nursing program graduated — the college successfully increased the amount of nurses completing their programs.
In spring 2021, the college graduated 44 ADN students and nine LPN students. In 2024, the college graduated 74 ADN students across the two cohorts and 13 LPN students.
For context, according to a recent NCBON report, 65% of nursing students statewide who started their final cohort in the 2022-23 academic year graduated, resulting in a 35% attrition rate.
The enrollment growth also allowed the college to bring in more state funding. By generating more FTEs from the nursing program expansion, Craven Community College is able to support the cost of the expanded program and no longer requires grant funding to support the nursing faculty salaries.
In addition to doubling the number of nursing student seats and generating more FTEs, the successful expansion of Craven Community College’s nursing program led to the college and health system partnering in various ways to increase the number of trained and skilled health care professionals across multiple areas.

Expanding the partnership
The success of the initial investments from CarolinaEast led to new partnerships between the college and health system. Below are some academic programs that have been created, expanded, or iterated as a result of this partnership.
Surgical technology
In 2023, CarolinaEast approached Craven Community College about their need for surgical technologists — those responsible for preparing operating rooms and helping surgeons and nurses during surgery.
Surgical technology is typically a two-year degree program, but Craven Community College decided to offer the program through workforce development. This allowed the college to expedite the process for setting up the program and meant students could finish in less than two years.
Now, the program consists of two 18-week courses that can be completed in approximately nine months. Graduates of Craven Community College’s surgical technology program are qualified for entry-level positions in surgical settings and are eligible to take the national certification examination for surgical technologists.
CarolinaEast provides a rotating suite of operating rooms for students, giving them practical, hands-on experience.
Licensed practical nurse
A hospital interest survey revealed that multiple CarolinaEast employees were interested in pursuing a licensed practical nurse (LPN) diploma, but they could not commit to a full-time program. A brainstorming session between CarolinaEast and Craven Community College leaders resulted in the creation of a part-time LPN program delivered on nights and weekends. Students enrolled in the nights and weekends LPN program can complete in two years. Craven Community College launched the program in fall 2024.
LPNs provide nursing care in a variety of settings, including home health agencies, physicians’ offices, and hospitals. Graduates of Craven’s LPN program are eligible to take the National Council Licensure Examination (NCLEX-PN), which is required to practice as a LPN.
Environmental services and housekeeping training
CarolinaEast and Craven Community College partnered in 2023 to provide environmental services (EVS) and housekeeping training. Students learn protocols for cleaning and disinfecting hospital rooms and health care facilities. They also receive instruction in time management, communication skills, and teamwork.
These positions are critical to hospital systems as they help prevent health care associated infections — protecting patients, visitors, and staff. Proper and effective EVS training can also significantly reduce wait times for patients.
The free EVS program is housed in the college’s workforce development training building, the Volt Center. A room inside the Volt Center was reconfigured to replicate a hospital room at CarolinaEast.
Students who complete the 64-hour program are guaranteed an interview with CarolinaEast.

Benefits
“How can we both give to get to a better place so that we can find an outcome that will be better for all of us?”
Dr. Jim Davis, chief nursing officer at CarolinaEast
The benefits of a partnership between a hospital system and academic institution are far-reaching.
Health systems
The partnership allows health systems to match academic programs to current vacancy needs, creating a wider pool of qualified candidates. Additionally, understanding employees’ desires for professional growth and working with the college to find solutions leads to increased hospital employee retention rates and transfers within the hospital system.
Academic institutions
The partnership enables colleges to respond more rapidly to the needs of the hospital and community. Program expansions have the potential to increase enrollment, generating more funding for the college.
Students and employees
Students and employees benefit from the partnership in numerous ways. Students are given real-world experience within the hospital system, and those planning to work at CarolinaEast are better prepared having trained on the hospital system’s equipment.
The partnership also connects employees with academic programs that meet their current professional development needs and wants. The hospital’s investment in current employees alleviates the financial burden of tuition cost.
Community
A fully staffed hospital reduces strain on the system and creates a more stable health care infrastructure for community members. Plus, growing local health care professionals establishes a health care system of professionals who live in the community where they work.

Key stakeholders
Sustaining this type of partnership takes commitment, willingness, ongoing communication, and the right people at the table.
“It’s a coordinated effort,” said CarolinaEast and Craven Community College leaders.
Key stakeholders and their roles include:
- Craven Community College
- Senior administration: Responsible for vision building, ongoing partnership communication, and community relationship building.
- Health sciences deans and directors: Responsible for program implementation and iteration, academic program problem-solving, and informing senior administration of changes.
- Nursing faculty: Provide academic instruction. Key support system for students.
- Public information officer: Develops ongoing messaging about hospital partnership, health care program opportunities, and community involvement.
- CarolinaEast Health System:
- Health system administration: Responsible for vision building, ongoing partnership communication, and community relationship building.
- Human resources: Implements changes to hiring requirements.
- Chief Nursing Officer: Identifies health care workforce needs, oversees clinical space scheduling, coordinates with the college regarding academic programming iterations.
- Director of Mission Effectiveness: Helps create professional development and growth culture within the hospital. Understands and communicates employees’ educational needs.
- Nursing Student Coordinator: The coordinator works closely with the college to secure clinical units for students’ clinical rotations. The coordinator also works with program directors to match students with preceptors during students’ capstone semester.
Alec Newton, dean of health programs at Craven Community College, highlighted the importance of the Director of Mission Effectiveness role at CarolinaEast:
“The Director of Mission Effectiveness did play a central role because she was a consistent driving force at CarolinaEast. She stayed in communication with their employees to keep the momentum going, kept management informed and involved, and worked through challenges with us to find solutions.”
Related reading
Lessons learned
“Start with one specific deal, you make good on it, and then everybody rushes to make the next deal.”
Dr. Ray Staats, president of Craven Community College
Through the years, Craven Community College and CarolinaEast continue to learn what makes a partnership between a college and hospital system successful.
Community colleges have long been heralded as the workforce engines of their communities. As such, a sustained partnership with a hospital system that is in need of qualified and skilled health care professionals is a no-brainer.
Staats said Craven Community College has been focused on working with CarolinaEast, and the college’s health care programs are built to meet the hospital’s needs.
Both groups should always try to get to yes, Staats said.
Michael Smith, CEO of CarolinaEast, said the college’s flexibility to help has been invaluable.
“Almost without exception, the community college has said, ‘Yes, we can help,’” Smith said.
Outlined below are key takeaways from interviews with administration, staff, and current students at Craven Community College along with leaders from CarolinaEast.
Over communicate
Communication is critical to building and sustaining partnerships.
While senior level leaders said they do not meet regularly, communication about organizational needs occurs naturally because leaders are active in the community and serve on various boards together.
The partnership has evolved in such a way that leaders responsible for implementing programmatic elements feel comfortable reaching out to each other to discuss issues or brainstorm solutions.
According to both organizations, the conversations are productive, stemming from a willingness to work together to solve needs — whether creating programs or adjusting hiring requirements.
Communication also flows beyond the organizations’ leaders.
The hospital sends messages to their employees about academic programs and professional development opportunities via email. However, hospital leaders said the best marketing seems to be word-of-mouth as current employees who are enrolled in college programs discuss the opportunities with other employees.
CarolinaEast and Craven Community College also hold informational sessions for current employees interested in pursuing academic programs at the college. The college helps employees understand the various pathways and time commitment required for different programs.
The communication from the college to the community consists of promoting health care programs and showcasing career trajectories. The college produces press releases about the partnership with CarolinaEast, and college advisors inform high school students about health care opportunities available to them through the college.
Relationships and presence matter
One strategic element is that of representation on both organizations’ boards.
Presently, Craven Community College’s chief academic officer sits on the board of CarolinaEast. The chief academic advisor has served in various roles at the college and previously worked as a nurse at CarolinaEast.
CarolinaEast’s chief nursing officer serves on the board of Craven Community College. Craven County commissioners appointed the CarolinaEast representative.
Cross-board representation allows both organizations to understand current needs and challenges. Additionally, the representation provides a pathway for creative problem solving between the two parties.
Before each graduation, the college holds a pinning ceremony to mark each nursing student’s transition to a professional nurse. It is a special moment for nursing students, highlighting their commitment.
In addition to Craven Community College leaders, a representative of CarolinaEast is present for those ceremonies. Both organizations’ leaders said it is important for the hospital to celebrate the accomplishments of students.
Hospital representatives have a chance to speak with students at the pinning ceremony who are undecided about their future employment.
When individuals see the strong partnership between the college and the hospital, it highlights both organizations’ commitment to serving the community and providing opportunities for employment and professional growth, said Judy Pierce, CarolinaEast’s mission effective coordinator.
Look for creative solutions to logistical challenges
Expanding the nursing program meant the college and hospital needed to work together to coordinate clinical space. In order to do this, the college had to adjust when they taught certain portions of the nursing program curriculum. To provide students in both ADN and LPN programs with a maternal-child clinical rotation and accommodate for clinical space, the college moved the maternal-child content portion to LPN’s third semester.
In its most recent iteration of the nursing program expansion, the college could no longer admit all students into the fall cohort. To accommodate 80 seats, the college started their first-ever spring cohort, opening 40 seats in the spring and 40 seats in the fall. The creation of a spring cohort allows the college the capacity to graduate 80 nursing students per year.
Expanding the nursing program and other health care programs meant the college had to consider how the growth would impact personnel.
The college created additional classroom and office spaces to accommodate the growth. The college also transitioned a part-time advisor to full-time, who is now responsible for advising all health care program students.

Recommendations
Below are recommendations for other colleges and health care systems to consider when scaling academic programs, providing resources, retaining health care professionals, and more.
Evaluate programs and hiring standards in high needs health care areas
Hospital leaders said the college’s willingness to evaluate its health care programs has been invaluable.
When the hospital was in need of surgical technology technicians, the college was quick to brainstorm solutions to expedite the program process.
The two-year surgical technology degree program was a roadblock for many students, but it was also a roadblock for the college and hospital. Developing a degree program takes about two years to start and then another two years to graduate students.
The hospital needed surgical technology technicians immediately.
After careful evaluation, it was determined the college could meet all accreditation standards by offering the program through workforce development. It takes about 90 days to go through approval and stand up a workforce development program, which is much faster than the time it takes to start a curriculum program. Staats said this approach means the college can “move at the speed of business.”
By offering the program through workforce development, students could graduate in nine months and be able to take the national certification examination, which gets students in the workforce sooner and reduces the cost to students significantly. For example, Newton shared that the surgical tech workforce development program costs about $920 for a student to complete in nine months compared to $9,400 for the two-year ADN program.
The change from a degree program to workforce development meant the hospital had to revamp their hiring process. An evaluation of the hospital’s requirements for surgical technology technicians eliminated the requirement of a two-year degree.
The college and hospital worked together to develop a program that would meet accreditation standards and the needs of the hospital, and hospital leaders praised the college for their ability to address workforce challenges while retaining high program standards.
Seek out additional funding
College leaders said philanthropic and grant funding can go beyond paying for nursing faculty salaries and benefits.
Community colleges enroll some of the most diverse student populations. Many of them are low-income, first-generation college students or adult learners, and they often experience financial, transportation, and child care challenges that can make academic success more difficult.
Leaders said additional funding could be used to:
- Cover tuition costs, particularly for students who do not qualify for tuition reimbursements from their employer or are ineligible for federal and state scholarships.
- Provide financial support for students who must work part-time to complete their nursing program. These funds could cover transportation, child care assistance, and other expenses associated with college attendance.
- Hire additional staff to help alleviate strain of expanding the college’s health care programs.
- Invest in the expansion of other high-need health care programs.
Generate interest in health care professions before high school graduation
During interviews, Craven Community College students shared that their decision to pursue a career in health care was made prior to high school graduation.
Two students discussed how a health seminar class in high school piqued their interest. Another student stated it was their parent’s involvement in the health care field that helped them make the decision. Each student expressed their overall desire to help people as the chief reason for choosing health care.
Their recommendation to hospitals and colleges is to connect with students as early as possible, showcasing nursing programs and careers in high-need health care areas. Students also said learning from hospital staff about available opportunities and advancement was critical.
Several students interviewed participated in North Carolina’s dual enrollment program, Career and College Promise (CCP), during high school. CCP provides structured opportunities for high school students to earn college credit tuition-free.
Students were able to complete nursing program prerequisites prior to their high school graduation through CCP.
“I did take advantage of (CCP) and was able to go directly into nursing classes,” said Clair Gatlin, a Craven Community College nursing student.
Completing courses like college-level math and anatomy and physiology allowed students to begin their nursing program almost immediately. Additionally, some students completed Nurse Aide I while still in high school, which is a program that teaches personal care for patients and is a requirement for the nursing program.
Evaluate efforts to retain hospital employees
Mitigating health care workforce shortages goes beyond hiring qualified employees. CarolinaEast’s mission effectiveness coordinator said retaining hospital employees is just as critical.
At CarolinaEast, employee retention strategies include providing professional development and opportunities for growth and advancement within the system.
Scholarship opportunities are provided based on the needs of the organization and “may be extended to employees as well as non-employees.” A work commitment is often required of employees who participate in these programs upon graduation.
The college and hospital coordinated a survey to identify academic program needs among hospital staff. Craven Community College created the survey, and CarolinaEast distributed the survey to employees.
The interest survey helped the hospital understand the areas in which employees desired professional development and transfer possibilities within the system. The college developed programs based on employee interest and the hospital’s workforce needs.
Surveying employees resulted in the college adding a nights and weekend cohort for the LPN program.
Additionally, the survey revealed the challenges and barriers hospital employees experience when pursuing an educational program.
Look for ways to partner beyond funding
This partnership extends beyond paying for nursing faculty salaries.
Expanding the nursing program meant the college needed at least two additional clinical space units. CarolinaEast worked with Craven Community College to create the units.
The hospital allowed students to train using the hospital’s technology system for patient records. Doing so provided students an opportunity to know the system before being hired by the hospital.
Additionally, the hospital designated operating suites for surgical technology students to train.
Assess programs and monitor outcomes
Continual assessment is critical. Craven Community College leaders said it is important to assess the quality of programs the college is providing and their outcomes.
Assessment includes ensuring the programs meet the needs of the current health care demand at the hospital. That requires partnering with the community’s health care system to ensure the skills and training needed are embedded in the college’s academic programs.
The college must also measure the outcomes of each program – ensuring graduates of each program are prepared and qualified for their intended careers.

What’s next
CarolinaEast and Craven Community College said the partnership will continue as needs are identified. Both organizations will problem-solve and find creative solutions to meet the demands of their community and the health care workforce.
Leaders are now discussing ways to partner beyond patient care to include areas such as technology, human resources, health information management, pharmacy technicians, and more.
These types of partnerships are growing across the state. Blue Ridge, Davidson-Davie, Durham Technical, Wayne, and Surry community colleges have launched similar partnerships with health care systems. For example, in 2024, Wayne Community College partnered with UNC Health Wayne to hire a clinical nursing instructor for a five-year period.
In addition to these partnerships, North Carolina Area Health Education Centers (NC AHEC) created a nursing clinical instructor partner program to increase nursing faculty. The program is a partnership between academic nursing programs and practice organizations, preparing qualified RNs to serve as clinical nursing instructors while still maintaining their role in a practice organization. The program is designed for RNs with a Bachelor of Science in Nursing (BSN) or higher who desire to work as a clinical instructor in an LPN, ADN, or BSN program.
These are just several examples of community colleges and health care systems partnering to address health care worker shortages. As Craven Community College President Dr. Ray Staats says, “Relationships are the magic of our system.”









