Over numerous cups of coffee in 2006, Dr. Kurt Michael and Angela Quick discussed an alarming statistic — the suicide rate in Watauga County was over 30% higher than the North Carolina average.
Dr. Michael, Stanley R. Aeschleman Distinguished Professor of Psychology at Appalachian State University, had an innovative idea for how to provide free mental and behavioral support to students at nearby public schools. Quick, then the principal of Watauga High School, was eager to collaborate.
The result was the Assessment, Support, and Counseling (ASC) Center, which is now available to almost 4,000 K-12 students at seven schools in three counties of western North Carolina.
“Our signature issue was suicide prevention,” says Dr. Michael on the origins of the university partnership. According to NC Child’s 2019 Child Health Report Card, suicide is the second leading cause of death for children ages 10 to 17. From 2008 to 2017, the statewide youth suicide rate nearly doubled. In 2017, 8.2% of North Carolina high school students attempted suicide.
The ASC Center went from an idea to a reality faster than one might expect. Dr. Michael and Quick, in cooperation with Watauga County Schools administrators, got the program up and running in the 2006-2007 school year.
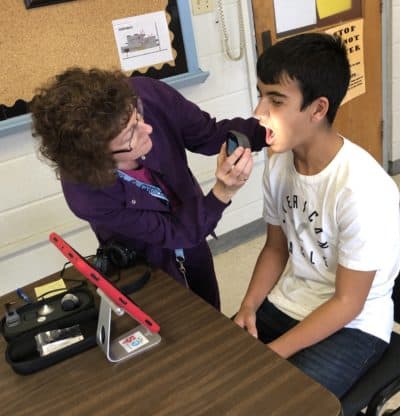
Following a medical school model, college students pursuing careers in psychology, counseling, and social work operate under the supervision of licensed clinicians to provide pro bono care to students who would otherwise have barriers to accessing mental health services. Dr. Michael describes the ASC Center’s mission as having three parts:
“To serve youth with effective mental health services in schools, that’s really number one. Number two is workforce development, trying to create the workforce to serve sustainable [mental health] systems. And third would be the research component.”
The first part of that mission would ideally be met by school counselors and school social workers, but many are overburdened by large caseloads and responsibilities that have little to do with the mental health of their students, such as arranging student schedules. The American School Counselor Association recommends a ratio of 250 students per school counselor. In North Carolina, the average caseload is 368. But in Alleghany, Ashe, and Watauga counties, trainees from the ASC Center are able to take on some of the most urgent cases, leaving school counselors better able to manage their regular caseloads. This benefits all students in schools served by the ASC Center, even those who do not use its services directly.
The ASC Center’s counseling services start with a referral. Anyone can make a referral, including teachers, friends, and students themselves. Dr. Michael gives this example, “If you’re a teacher and you make an observation, you might come to a school counselor and say, ‘I’ve got this kid that I don’t know what’s going on at home, but I’m concerned,’ and it comes from a place of compassion.”
Upon receiving a referral, a school counselor or social worker coordinates between the student and the ASC Center, managing intake and consent forms. That person then presents the student’s case to representatives from the ASC Center at a weekly meeting which takes place at each of the seven schools served by the ASC Center. The ASC Center then sets up a meeting with the student, the counseling trainee assigned to the case, the licensed clinician overseeing the trainee’s work, and other stakeholders.
“We collaborate with the departments of social services, with law enforcement, with juvenile justice. We’re trying to be that connector, that support system for students,” explains Dr. Michael. Together, they develop a treatment plan customized for that individual student. From that point on, the trainee and student meet regularly according to the treatment plan, with the trainee reporting to the licensed clinician and stakeholders as appropriate.
To pay for the program, each participating district contributes $20,000 to $30,000 annually. These payments help cover the costs of research assistants, operational funds, and having the clinicians from App State reassigned to the program from university classrooms. For this amount, a district wouldn’t even be able to hire a single school counselor. Additional funding for the program comes from grants, including a recent one from the American Foundation for Suicide Prevention.
A major challenge in measuring outcomes for school-based health programs is the inability to merge health data (protected by HIPAA) with educational data (protected by FERPA). This makes it virtually impossible to show whether improved access to healthcare has an impact on student learning.
But those barriers are not present for students who consent to receive care from the ASC Center. The consent forms signed by students and guardians grant the ASC Center access to both HIPAA- and FERPA-protected data. As a result, App State students and faculty are able to conduct research on the efficacy of their practices, a rarity among school health initiatives.
For Dr. Michael and his researchers, protecting privacy is a high priority. “We never share individual data, always aggregate. We communicate with the students and the parents [or guardians] about their individual responses to treatment, but that’s never, ever shared beyond them.”
According to the ASC Center’s website, in 2011-2012 it served 64 students directly, 54% of whom improved their academic performance and 74% of whom increased their attendance and decreased their disciplinary incidents. A 2013 study found that students who were referred to the ASC Center improved or recovered from “clinically significant” symptoms 63% of the time.
In 2019, the ASC Center (in partnership with Ashe County Schools and RTI International) received a $2.5 million, five-year grant from the Department of Education. This grant will enable them to continue to expand mental health services and training in rural North Carolina. The ASC Center plans to expand services in the three counties where they already operate.
Dr. Michael sees this model as being replicable elsewhere. “I’ve actually been asked to help programs around the nation, here and there, so we try to disseminate the idea to other states, and with some success.”
The Department of Education grant opens the door to future expansion across the state, as does recent statewide legislation. On June 8, 2020, Governor Roy Cooper signed into law Senate Bill 476:
“An act to require the State Board of Education to adopt a school-based mental health policy and to require K-12 school units to adopt and to implement a school-based mental health plan that includes a mental health training program and a suicide risk referral protocol.”
From Dr. Michael’s perspective, “The language is inspiring, but mostly it’s aspiring,” because there is no funding attached. But he’s hopeful that the passage of this bill will encourage more districts and mental health providers to establish collaborations like the ASC Center, and ultimately reduce suicide rates in North Carolina.
This article is part of a series on innovative approaches to health in schools. Find the rest of the articles here. For more on youth suicide, see EducationNC’s five-part series here.