
|
|
During a year in which lawmakers are saying there may not be funding for raises, the State Health Plan’s Board of Trustees took the first step on Friday to set premiums for active members based on a salary scale. Increases in premiums are likely for all educators, according to the discussion by the Board, and Friday’s vote may mean veteran educator premiums increase even more.
The vote was part of a larger discussion on the health plan’s structure and strategies to “avoid a looming fiscal crisis,” according to a Board press release.
“Despite increased funding from the state, the Plan is facing a $507 million deficit, which is estimated to grow to $1.4 billion by 2027,” the press release said. “The Plan has been spending more than it has been bringing in, and it’s out of cash reserves to help bridge the financial gap.”
On Jan. 1, Aetna became the State Health Plan’s third-party administrator, after the Board voted in December 2022 to switch from its long-term administrator, Blue Cross Blue Shield, which administered the plan for more than 40 years.
When the plan’s transition was first announced, former state treasurer Dale Folwell said that none of the benefits or costs would change for plan members. However, on Friday, state officials said some changes were necessary for the plan to remain financially solvent.
“The budget can’t be balanced without changes,” said Chief Economist Dr. Emma Turner.
The plan provides health care coverage to nearly 750,000 teachers, charter school employees, community college employees, other state employees, retirees, and dependents, according to the website.
According to the Board’s press release, “the goal of the tiered premiums is to make coverage more affordable for Plan members at lower salary levels.”
Friday’s vote did not approve actual premiums, but gave the Board the authority to set premiums based on salary tiers. Executive Administrator Tom Friedman said that any vote to determine actual premium rates would take place at some point during the summer. The Board hopes to present specific timeline goals at its March meeting, he said.
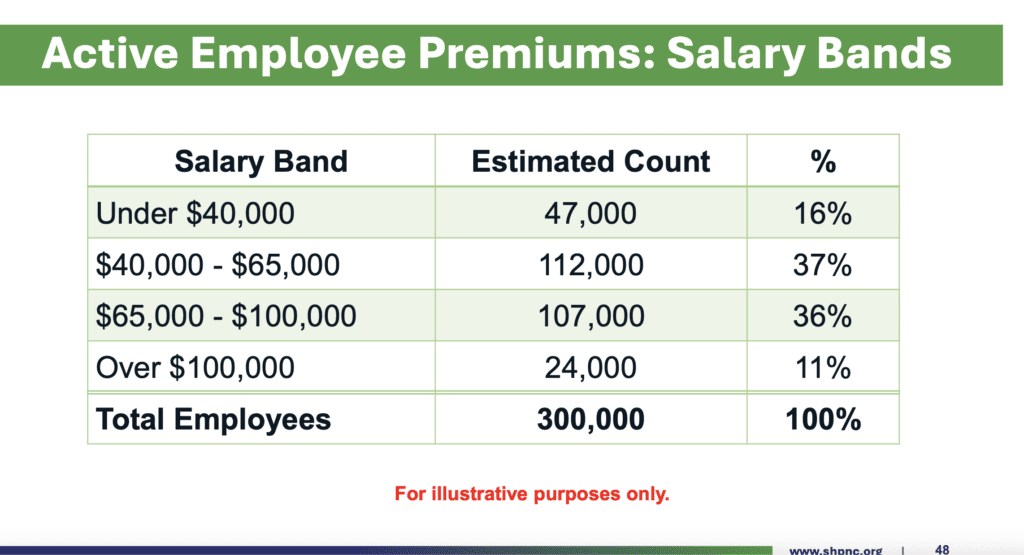
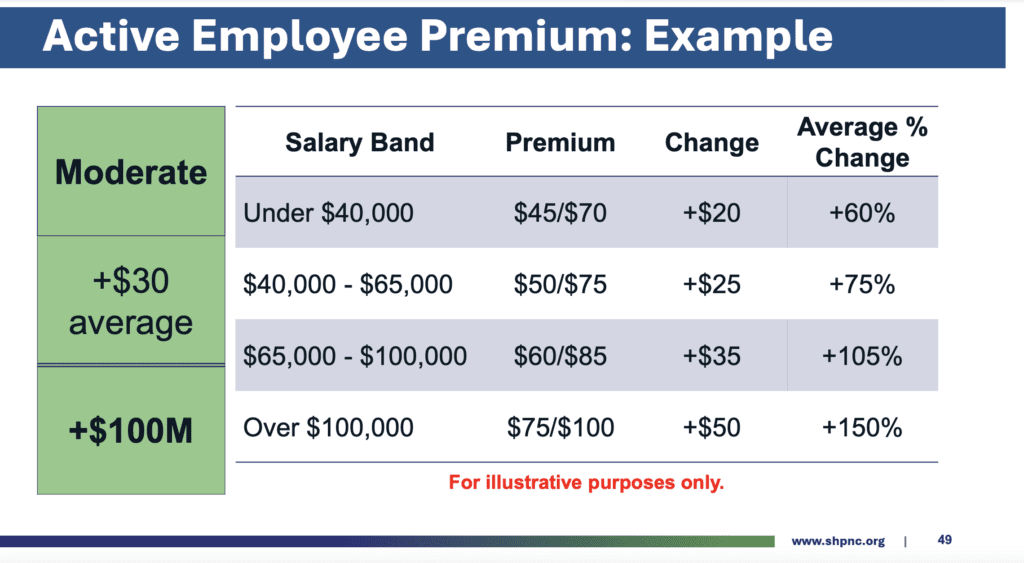
Here’s a look at the initial moderate example changes the Board discussed on Friday, along with a look at how many employees are estimated to be in each salary tier.
During a brief public comment period, speakers questioned why a deficit in the health care plan must be paid by employees, rather than by health care providers or the state.
North Carolina Association of Educators (NCAE) President Tamika Walker Kelly said asking teachers to pay more for health care will lead to more teachers and staff deciding to leave schools.
“We cannot afford the risk of pricing our educators out of the profession,” she said. “Our crisis was created by state lawmakers who have failed to provide salaries that meet the rising costs that we are all dealing with. And therefore, I say it is the state lawmakers who should pay to close the health care gap, not our school employees.”
The rates discussed on Friday are only examples, state Treasurer Brad Briner said. The Board will continue its discussion about how and if to implement premiums based on salary tiers in the coming months, before voting on any changes during the summer.
“If the Board elects to go back to one premium rate, that would be workable under this structure,” the Board’s presentation says.
Now that the Board approved the plan’s ability to implement tiered premiums, the treasurer’s office must research how much the technology to do so would cost. Before the Board’s March meeting, the office will also run projections on savings if premiums were only increased for employees making more than $65,000 a year, per the request of a Board member.
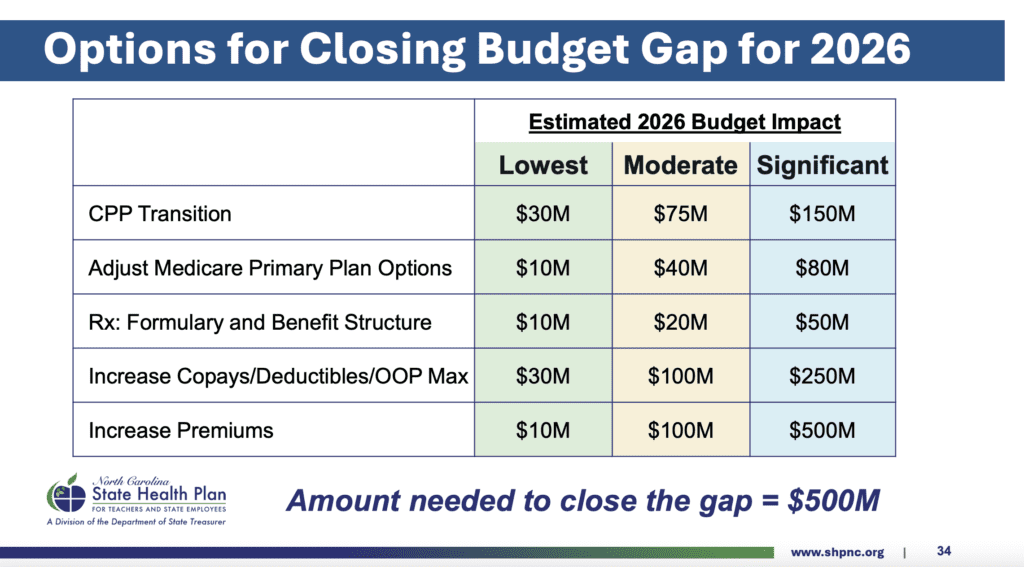
The Board also discussed several other options for closing the budget gap in 2026, including changes to the Clear Pricing Project (CCP), adjustments to Medicare primary plan options, prescription structures, and increasing copays/deductibles and Out-of-Pocket maximums.
In the table below, you can see the estimated impact of low, moderate, and significant changes in each category.
“We’ve got to do something between moderate and significant in some of these areas to close that gap,” Friedman said. “The goal is long-term sustainability and not making changes we can’t go backwards on.”
You can view the Board’s full presentation here; see slides 48-54 for information on the salary-based premium changes.
Implementation of switch to Aetna
Even before changing premiums, some members have seen increases in out-of-pocket expenses for medical services covered by the state health plan, according to reports received by the NCAE.
“It varies from individuals sharing that they are now paying fees that they didn’t have before for prescription medicine, or co-pays that they didn’t have to pay before for visits they’ve done plenty of times over the years,” Walker Kelly told WUNC. “… The state health plan is one of the remaining benefits that our educators here in North Carolina depend on. That is why this one feels particularly pointed for our educators.”
According to the WUNC report, Briner said the problems are due to the application of the Clear Pricing Project, which allows members to choose health care providers who offer transparent pricing to the state in exchange for lower co-pays for patients.
Briner said all providers in the Clear Pricing Project (CCP) had to re-enroll this year to remain in the program this year, unlike previous years.
“In the context of the transition from Blue Cross to Aetna, it has come to our attention that some providers meant to sign up for CPP again and did not complete (it) for one reason or another,” Briner told WUNC.
On Friday, Briner said CCP has cost the state too much. The presentation to the Board said the program is “being reassessed to strike a balance between improving member health, financial sustainability, and provider quality.”
He said his office is working with Aetna to solve any issues arising from the transition.
“Implementation is going well, but there are bumps,” Briner said about the switch to Aetna. “We acknowledge that and we are working to correct them, and we are very grateful for (Aetna’s) continued partnership and support… and for the staff (who) has been working around the clock, fielding challenges, fielding questions.”
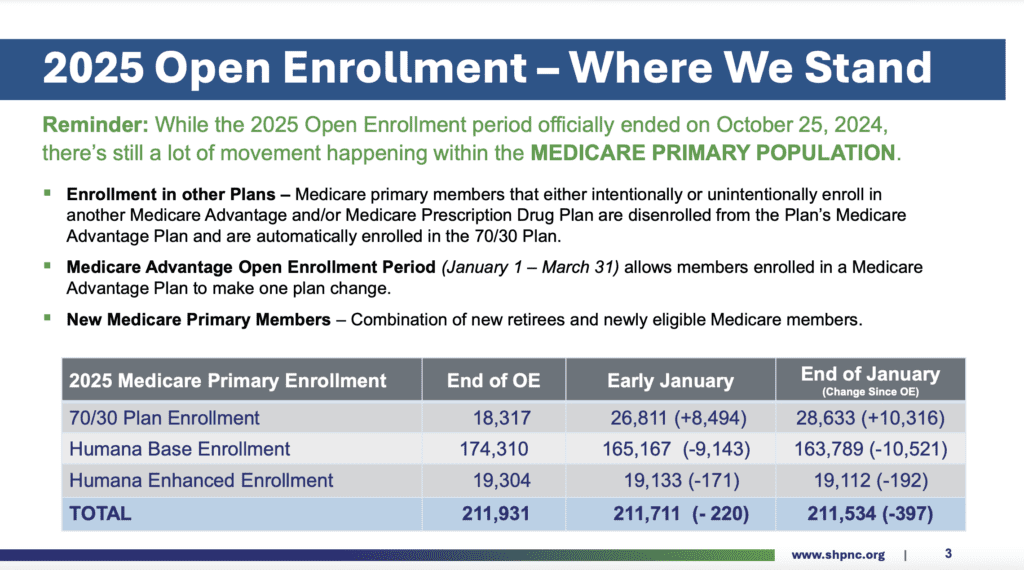
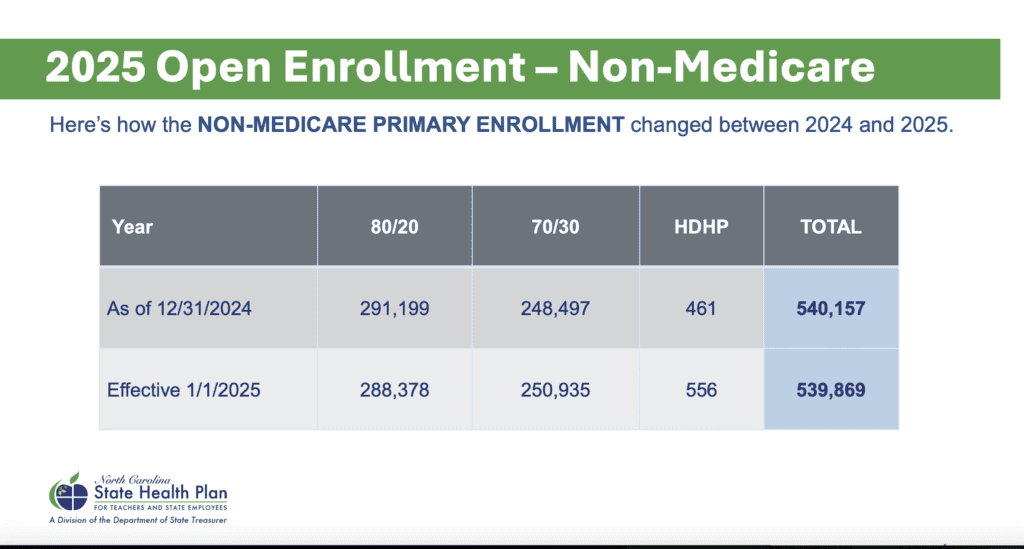
Here’s a look at the open enrollment data presented on Friday.
More on the State Health Plan Board Board of Trustees
The State Health Plan’s Board of Trustees has 10 members. According to the Board’s website, “the board is made up of experts in medicine, health administration and education and is responsible for the design of employee health benefits.”
Here are the members of the Board:
- Treasure Brad Briner, chair and ex-officio member.
- Kristin Walker, state budget director of North Carolina and leader of the Office of State Budget and Management (OSBM). Walker was appointed by the governor in 2022.
- Dr. Brian Miller, a practicing hospitalist at the Johns Hopkins Hospital, professor at the Johns Hopkins University School of Medicine, and a nonresident fellow at the American Enterprise Institute. Miller is a treasurer appointee.
- Mike Stevenson, whose 43-year health care career includes working as chief financial officer for Halifax Memorial Hospital in Roanoke Rapids and Murphy Medical Center’s chief executive officer. Stevenson was appointed by the speaker of the House.
- Cyrus Vernon, former instructor at Caswell County Schools for 34 years, is also a speaker appointee.
- Sam Watts, was named executive director of the North Carolina Retirement Systems by Briner in January 2025. Watts previously was executive director of the State Health Plan from 2022-24. He was appointed to the board by the treasurer.
- Melanie Bush, the deputy Medicaid director for the North Carolina Division of Health Benefits, was appointed by the governor.
- Wilton Russell “Rusty” Duke, Jr., “is engaged in a broad criminal and civil litigation practice for the firm of White and Allen. He has served as the Senior Resident Superior Court Judge of Pitt County, Resident Superior Court Judge and as a District Court Judge of Pitt, Craven, Carteret and Pamlico Counties.” Duke is a Senate appointee.
- Dr. Kerry Willis is a practicing physician at Open Water Medical PA, which he founded. He serves as chairman of the Atlantic Integrated Health Physicians Organization, “which he helped found in 1995 to give physicians a better voice in design and delivery of health care services in eastern North Carolina,” per the Board’s website. Willis was appointed by the Senate.
- Kimberly Jones, 2023 Burroughs Wellcome Fund North Carolina Teacher of the Year, is an English and Humanities teacher for Chapel Hill Carrboro City Schools. She was appointed by the governor.
You can contact members of the Board via email at SHPBoard@nctreasurer.com.




